Root Debridement
What is Periodontal Disease?
Periodontal disease (advanced gum disease) is a chronic inflammatory condition affecting the supporting structures of teeth, including gums, periodontal ligament, and alveolar bone.
It’s primarily caused by plaque accumulation that hardens into calculus (tartar) if not removed.
The disease progresses from gingivitis (gum inflammation) to periodontitis, which can lead to irreversible damage such as bone loss and tooth loss.
Symptoms of Periodontal Disease
Early Stage (Gingivitis):
- Red, swollen, or tender gums
- Bleeding during brushing or flossing
- Persistent bad breath (halitosis)
Moderate to Advanced Stage (Periodontitis):
- Receding gums or teeth appearing longer
- Loose or shifting teeth
- Pain while chewing
- Pus between teeth and gums
- Deep periodontal pockets
- Bone loss
Causes of Periodontal Disease
The primary cause is poor oral hygiene, allowing plaque to accumulate. Other contributing factors include:
- Lifestyle factors: Smoking, poor diet, stress
- Systemic conditions: Diabetes, cardiovascular disease, autoimmune disorders
- Hormonal changes: Pregnancy, puberty, menopause
- Medications: Drugs reducing saliva flow (antihistamines, antidepressants)
- Genetic predisposition: Family history
Diagnosis Methods
A dentist diagnoses periodontal disease through:
- Clinical examination: Assessing gum health, measuring pocket depth, checking for bleeding
- X-rays: Evaluating bone loss around teeth
- Periodontal probing: Using a calibrated probe to measure periodontal pocket depth
Treatment Options
Treatment depends on severity:
- Scaling and Polishing: For mild cases, removes plaque and calculus above and below gum line
- Root Planing (Deep Cleaning): For moderate cases, smooths root surfaces to remove bacteria
- Surgical Treatment: For severe cases, may include flap surgery, bone grafting, or guided tissue regeneration
Difference between scaling and root debridement
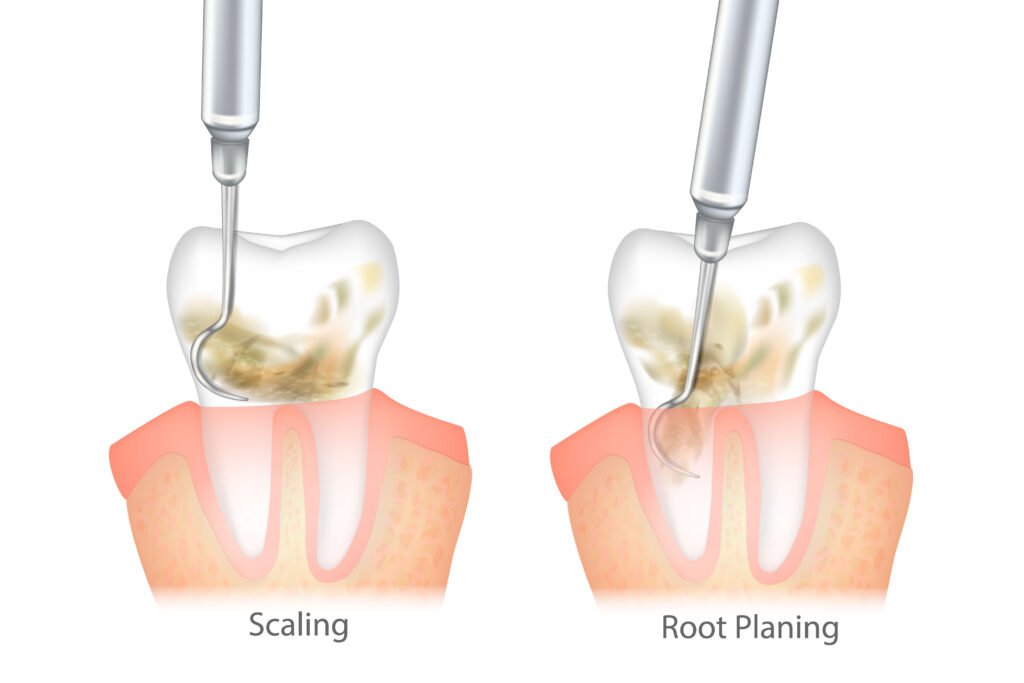
Scaling removes plaque and calculus from tooth surfaces.
Root debridement involves more thorough cleaning of root surfaces to remove bacterial toxins and infected tissue to promote healing and gum reattachment.
FAQs About Periodontal Disease
Yes, through:
- Brushing twice daily with a soft-bristled toothbrush and fluoride toothpaste
- Flossing daily to remove plaque between teeth
- Regular dental check-ups every 6-12 months
- Using antibacterial mouthwash to reduce bacteria
- Avoiding smoking and managing conditions like diabetes
Gingivitis is reversible with proper treatment and improved oral hygiene. However, periodontitis can only be managed to prevent further damage, as lost bone and tissue cannot fully regenerate.
Periodontal disease is linked to:
- Diabetes: Makes blood sugar control harder; diabetes increases infection risk
- Cardiovascular disease: Bacteria can enter bloodstream, contributing to arterial plaque
- Respiratory infections: Inhaling oral bacteria can lead to lung infections
- Pregnancy complications: Associated with preterm birth and low birth weight
Most treatments use local anesthesia to minimize discomfort. After treatment, patients may experience mild sensitivity, soreness, or swelling that typically subsides within days. Pain management medications can help.
While good oral hygiene is essential, professional treatment is necessary for removing calculus from deep pockets. Home care alone cannot address advanced periodontal disease.
Non-surgical treatments like scaling and root planing can be completed in 1-2 sessions.
Surgical treatments may require multiple visits.
Regular follow-ups are essential to monitor progress.
Untreated disease can lead to:
- Severe gum recession and bone loss
- Tooth loosening and eventual tooth loss
- Chronic pain and difficulty chewing
- Increased risk of systemic health issues
Yes, smoking is a major risk factor as it weakens the immune system, reduces blood flow to gums, impairs healing, and makes treatment less effective.
Yes, non-surgical treatments like scaling, root planing, and laser therapy can effectively manage mild to moderate periodontal disease. Advanced cases may still require surgery.
Yes, periodontal disease can recur if proper oral hygiene and regular dental visits are not maintained. Patients with a history of periodontal disease should be especially vigilant.
Diabetes increases risk by impairing blood flow, reducing the body’s ability to fight infections, and delaying healing. Conversely, periodontal disease can make it harder to control blood sugar levels.
Yes, advanced periodontal disease can destroy the supporting structures of teeth, leading to tooth loosening and eventual loss.
Genetics can influence susceptibility to periodontal disease. Certain genetic markers are associated with increased inflammation and higher risk of gum infections.
Yes, stress can weaken the immune system, increase inflammation, and reduce the body’s ability to fight infections. It may also lead to poor oral hygiene habits.
Quick Links
Contact
- +852 9532 1766
-
Room 1605, Island Beverley Center,
No. 1 Great George Street, Causeway Bay, Hong Kong
©DR. ROMAINE NG, All Rights Reserved