深層清潔
什麼是牙周病?
牙周病(中晚期牙齦疾病)是一種慢性炎症性疾病,影響牙齒支持組織,包括牙齦、牙周膜和牙槽骨。
它主要由牙菌膜積聚引起,如不清除會硬化成牙結石。
疾病從牙齦炎(牙齦發炎)發展為牙周炎,可導致不可逆損害,如骨質流失和牙齒脫落。
牙周病症狀
早期階段(牙齦炎):
- 牙齦紅腫或疼痛
- 刷牙或使用牙線時出血
- 持續口臭
中晚期階段(牙周炎):
- 牙齦萎縮或牙齒變長
- 牙齒鬆動或移位
- 咀嚼時疼痛
- 牙齒和牙齦間有膿液
- 形成深層牙周袋
- 骨質流失
牙周病成因
主要成因是口腔衛生不佳,導致牙菌膜積聚。其他因素包括:
- 生活方式:吸煙、不良飲食、壓力
- 全身性疾病:糖尿病、心血管疾病、自身免疫性疾病
- 荷爾蒙變化:懷孕、青春期、更年期
- 藥物:減少唾液分泌的藥物(抗組胺藥、抗抑鬱藥)
- 遺傳傾向:家族牙周病史
診斷方法
牙醫通過以下方式診斷:
- 臨床檢查:評估牙齦健康,測量牙周袋深度,檢查出血情況
- X光檢查:評估牙齒周圍骨質流失
- 牙周探測:使用校準探針測量牙周袋深度
治療選項
治療取決於嚴重程度:
- 洗牙和拋光:輕微病例,清除牙齦線上下方的牙菌膜和牙結石
- 牙根刮治(深層清潔):中度病例,平滑牙根表面以去除深層牙周袋中的細菌
- 手術治療:嚴重病例,可能包括翻瓣手術、骨移植或引導組織再生
洗牙和深層牙根刮治的區別
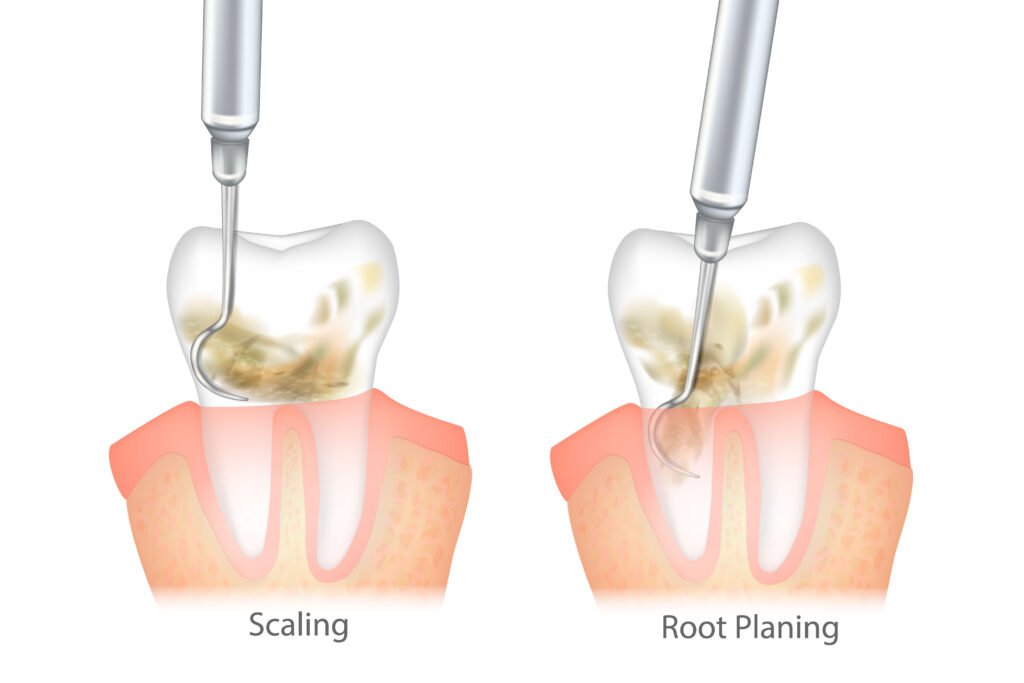
洗牙去除牙齒表面的牙菌膜和牙結石。
深層清潔則更徹底清潔牙根表面,去除細菌毒素和受感染組織,促進癒合和牙齦重新貼附。
牙周病常見問題
可以,通過:
- 每天刷牙兩次使用軟毛牙刷和含氟牙膏
- 每天使用牙線清潔牙縫
- 每6-12個月定期牙科檢查和專業清潔
- 使用抗菌漱口水減少細菌
- 避免吸煙並管理糖尿病等疾病
牙齦炎可以逆轉,但牙周炎只能控制預防進一步損害,已失去的骨質和組織無法完全再生。
牙周病與以下疾病有關:
- 糖尿病:使血糖控制更困難;糖尿病增加感染風險
- 心血管疾病:細菌可進入血液,導致動脈斑塊
- 呼吸道感染:吸入口腔細菌可能導致肺部感染
- 妊娠併發症:與早產和低出生體重有關
大多數治療使用局部麻醉減少不適。治療後可能出現輕微敏感、酸痛或腫脹,通常幾天後會消失。止痛藥可幫助緩解不適。
雖然良好的口腔衛生很重要,但必須進行專業治療清除深層牙周袋中的牙結石。家庭護理無法治療晚期牙周病。
非手術治療如洗牙和牙根刮治通常需要1-2次診療。手術治療可能需要多次診療。定期覆診對監測病情進展至關重要。
未經治療的疾病可導致:
- 嚴重牙齦萎縮和骨質流失
- 牙齒鬆動和最終脫落
- 慢性疼痛和咀嚼困難
- 增加全身健康問題風險
是的,吸煙是主要風險因素,它會削弱免疫系統,減少牙齦血液供應,影響癒合,並降低治療效果。
是的,非手術治療如洗牙、牙根刮治和激光治療可有效管理輕度至中度牙周病。嚴重病例可能仍需手術治療。
是的,如果沒有保持良好的口腔衛生和定期牙科檢查,牙周病可能會復發。有牙周病史的患者應特別注意口腔護理。
糖尿病增加風險,因為它會影響血液供應,降低身體抵抗感染的能力,並延遲癒合。相反,牙周病也會使血糖控制更加困難。
是的,晚期牙周病會破壞牙齒的支持結構,導致牙齒鬆動和最終脫落。
遺傳可能影響易感性。某些基因標記與增加炎症和牙齦感染風險有關。
是的,壓力會削弱免疫系統,增加炎症,降低身體抵抗感染的能力。它還可能導致不良的口腔衛生習慣。
Contact
- +852 9532 1766
- 香港銅鑼灣記利佐治街1號金百利中心1605室
Opening Hours
© 2025 DR. ROMAINE NG, All Rights Reserved